Acetylcholine is a major neurotransmitter found throughout the human body. Modulating its activity by either promoting or blocking its effects can manifest in many ways. The collective effects seen when acetylcholine activity is blocked is referred to as an "anticholinergic" effect.
As consultant pharmacists, we are always on the lookout for adverse medication effects in our patients. Anticholinergic side effects top the list of things we typically look for. These side effects can manifest in many ways including dry mouth/eyes, blurred vision, worsening glaucoma, increased heart rate, urine retention, constipation, headaches, confusion, cognitive impairment, and delirium. Such side effects can be very troublesome, especially in the elderly. Outcomes of anticholinergic side effects often lead to prescribing cascades and ultimately to more medications than necessary. More serious outcomes could include falls, fractures, urgent care visits, and hospital admissions.
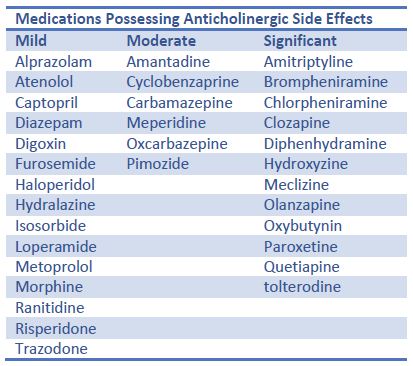
There are common medications that we typically associate with anticholinergic effects such as over-the-counter cold and allergy preparations that contain antihistamines such as diphenhydramine, chlorpheniramine, etc. These medications are widely used and have powerful anticholinergic activity. As we focus on these big offenders we may sometimes overlook less obvious medications that have less powerful effects. Many older patients take multiple medications to treat different chronic conditions. Some very common medications possess slight to moderate anticholinergic activity. While individually, medications with low anticholinergic activity may not lead to an overt side effect, several of them prescribed together could cumulatively lead to a significant side effect indeed. The concept of the additive anticholinergic activity of multiple medications contributing to a significant side effect is known as the anticholinergic burden. Examples of some of the more common medications we see prescribed in our patients can bee seen in the table along with their relative contributions to anticholinergic burden.
When we review patients for anticholinergic side effects we usually think of the negative outcome as an immediate side effect or acute negative impact on cognitive function. Newer evidence suggests that a chronic anticholinergic burden might have long term effects on cognition and may even increase the risk for death in elderly patients. Those who already have some degree of memory/cognitive impairment seem to be especially vulnerable to these long term risks. Patients with no overt manifestation of anticholinergic side effects may still be at some long term risk if their anticholinergic burden is high. As consultant pharmacists we must pay attention to our patients' anticholinergic burdens and attempt to keep them as low as clinically feasible. Doing so not only minimizes the risks for medical complications now but may also protect them from hastened cognitive decline for years to come.